Diabetes
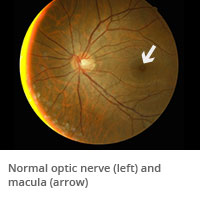
Annual eye exams for people with diabetes are important. Diabetes is the result of elevated blood sugar levels, which damage blood vessels everywhere in the body, including the eyes. Because the eye is such a small organ, damage to blood vessels in the eyes often occurs earlier than in larger organs like the heart and kidney.
What is diabetic retinopathy?

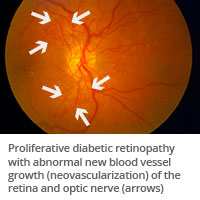
Background retinopathy is often a precursor to proliferative diabetic retinopathy, a more advanced and serious form of diabetic retinopathy. With proliferative retinopathy, blood vessels are so damaged that they become blocked. As a result, the retina doesn't receive the oxygen it needs so it starts to grow new blood vessels. These new blood vessels are abnormal and fragile. They grow above the surface of the retina where they are highly susceptible to bleeding.
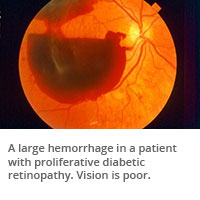
When bleeding occurs, blood fills the inside of the eye and prevents light rays from reaching the retina. Vision loss may be experienced as black spots or in the case of a larger hemorrhage, almost total loss of vision. Sometimes these blood vessels will also cause scar tissue to grow. The scar tissue shrinks and wrinkles and pulls on the retina and causes distorted vision. If the retinal traction is extreme, the retina can detach resulting in vision loss.
How is diabetic retinopathy treated?
Medications administered into the eye can be used to treat swelling, called macular edema. Laser surgery can help seal abnormal, leaky blood vessels and reduce the risk of bleeding. If the blood does not clear within a reasonable time, or if a retinal detachment is detected, an operation called a vitrectomy can be performed to remove the hemorrhage and to treat the abnormal blood vessels.
People with proliferative diabetic retinopathy sometimes have no symptoms until it is too late to treat them. The retina may be badly injured before there is any change in vision. Careful monitoring and control of blood sugar decrease the chance of developing proliferative retinopathy.
How often should I have an eye exam?
Patients with diabetes should have regular eye exams, as recommended by the American Academy of Ophthalmology:
- For patients with a normal eye exam or mild background retinopathy, follow up with an eye exam every 6-12 months.
- For patients with severe background retinopathy or proliferative retinopathy, follow up with an eye exam every 2-4 months. The presence of macular edema may shorten these intervals.
- Finally, women with diabetes who become pregnant experience a higher risk of developing diabetic retinopathy because of changes in metabolism. They are encouraged to have their eyes examined prior to conception and again during the first trimester.
The doctors at University Eye Specialists help you create an integrated treatment plan to prevent, slow, and manage diabetic retinopathy.
Back to top